The pelvic floor
There is a good chance you’ve never thought about your pelvic floor, let alone know its function and how to locate it within your own body. Maybe you have heard of Kegel exercises, but there it likely ends.
As physiotherapists, our world looks different. We deal with a broad range of musculoskeletal conditions, and knowledge about pelvic health should fall within that range. However, pelvic health is still taboo in our clinical practice, and little funding has gone into research on pelvic health in athletes and postpartum return-to-sports so far.
During a physiotherapist’s basic education, learning about pelvic health and dysfunctions is uncommon unless you study to become a pelvic floor specialist. It is almost as if the pelvic floor is separate from the rest of our body, which is surprising, if not shocking, considering that the pelvic floor is as much of a part of the musculoskeletal system as any other body part and plays a crucial role in daily tasks, pregnancy, birth, and sports.
At Movement Based Therapy, we want to change this paradigm and take matters into our own hands by educating ourselves and our patients about pelvic health, pregnancy and postpartum management to promote better care and decisions throughout your journey.
What is pelvic health, where is the pelvic floor, and what is pelvic floor dysfunction?
Pelvic health is the functioning and management of the reproductive organs, bladder, and bowels. We are looking at dysfunctions and the close interplay between these organs, which are supported by the pelvic floor.
The pelvic floor is defined as a floor of muscles which spans between the tailbone (coccyx) and pubis. Muscle bands, ligaments and connective tissue surround the reproductive organs, urethra and anus to make sure that voluntary function can be performed (Peinado-Molina et al., 2022).
Pelvic floor dysfunction (PFD) can affect both males and females but is especially prevalent in pregnant and postpartum women. Further risk factors associated with PFD include smoking, obesity, surgery to the pelvic floor organs, menopause and connective tissue disorders. Symptoms of dysfunction include involuntary loss of urine or faeces, having a strong urge or difficulties emptying the bladder, heaviness around the vagina or problems in sexual functions (Kenne et al., 2022). In males, pelvic floor dysfunctions can show as incontinence, organ prolapse or erectile dysfunctions.
The latest research on pelvic floor health in athletes
Whilst the awareness and discussion around pelvic health and pelvic floor dysfunctions has started to pick up, the field has long been an underfunded and under-recognised area. The reasons vary from female athletes not knowing how to address their complaints to sports clinicians not knowing how and what to ask about pelvic floor dysfunctions or that problems could even occur in female athletes (Dakic et al., 2021).
Therefore, researchers within the field of pelvic health advocate that knowledge and screening of pelvic floor dysfunction in sports should not be limited to pelvic floor specialists but made accessible to general medical professionals, coaches and staff treating athletes – and they could not be more right. The ‘PFD-SENTINEL’ was developed out of this demand: a screening tool to guide female athletes to a referral to pelvic floor specialists if needed. This tool is an excellent example of how every good care starts with the right questions asked. Ultimately, this questionnaire should be used by professional and recreational athletes (Giagio et al., 2023).
Pelvic health and sports
In 2022, the Welsh Rugby Union started a ground-breaking study to evaluate stress urinary incontinence (SUI) and the impact rugby has on the pelvic floor. The goal was to keep female athletes on the playing field by providing tailor-made pelvic floor exercise programs. The study found that load and demands on the pelvic floor differ hugely, depending on a player’s field position. Front rows had a higher load on their pelvic floor than back rows due to higher impacts and tackles with other opposing teams (Jones, 2022).
The IOC (International Olympic Committee) has recently made great efforts to implement screening questions for pelvic floor dysfunctions into their standard injury screening protocols. These efforts were displayed widely during the 2024 Summer Olympics, where pre- and postnatal mothers participated in their discipline like never before in the Olympic Games.
Return-to-sports postpartum
The pelvis and its muscles undergo significant changes and efforts with pregnancy and birth. The further into pregnancy, the higher the demands on the lower back, the abdominals and the pelvic floor muscles. Additionally, the pregnancy hormone relaxin plays a crucial role during pregnancy. Its function is to loosen the soft tissues such as ligaments, muscles and tendons in preparation for birth, which can also increase the risk of sports injury during pregnancy and in early post-partum stages. Research has also shown that relaxin supports soft tissue remodelling and healing, which is incredibly important after having gone through birth (Ng et al., 2015).
Knowing this information highlights the importance of structure for return-to-sports for young mothers in professional and recreational sports. This multidisciplinary approach should include sports clinicians, midwives, and physiotherapists. Out of this need, Donnelly et al. created the ‘6R Framework’; its design supports physiotherapists and coaches to guide female athletes safely back into sports post-partum. The framework highlights, in particular, the importance of a whole-system approach, addressing the mother and baby’s physical, social and psychological well-being (Donnelly et al., 2022). For more information, please read the infographic.
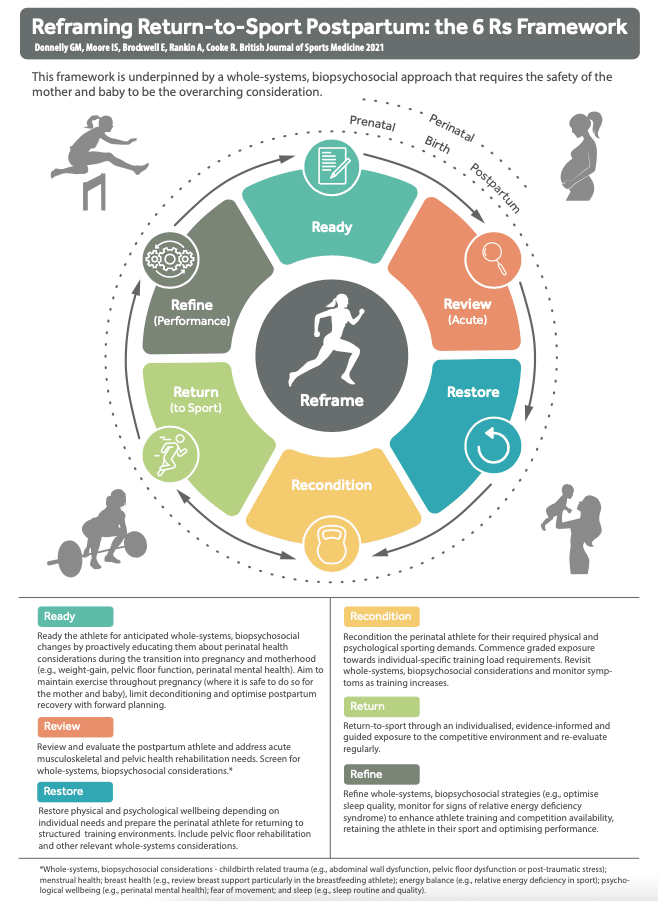
The ‘6R Framework’ by Donnelly et al. (2022) is a clever and comprehensive tool that helps both physiotherapists and clients work in a structured and holistic setting, two attributes we stand for at Movement Based Therapy. We aim to use this framework to guide you through your transition into motherhood, refer you to our colleagues who are pelvic floor specialists if needed, and safely return you to sports post-partum.
References:
- Dakic J, Hay-Smith J, Cook J, et al. Screening and management of pelvic floor symptoms in exercising women: online survey of 636 health and exercise professionals [Congress presentation abstract]. International Continence Society (ICS) Congress 2021. Available: https://www.youtube.com/watch?v=wC_JS32mGI8 ;
- https://www.ics.org/2021/abstract/52
- Donnelly, G. M., Moore, I. S., Brockwell, E., Rankin, A., & Cooke, R. (2022). Reframing return-to-sport postpartum: the 6 Rs framework. British journal of sports medicine, 56(5), 244–245. https://doi.org/10.1136/bjsports-2021-104877
- Giagio, S., Salvioli, S., Innocenti, T., Gava, G., Vecchiato, M., Pillastrini, P., & Turolla, A. (2023). PFD-SENTINEL: Development of a screening tool for pelvic floor dysfunction in female athletes through an international Delphi consensus. British journal of sports medicine, 57(14), 899–905. https://doi.org/10.1136/bjsports-2022-105985
- Jones, L., Welsh Rugby Union, 2022, available on: https://www.wru.wales/2022/03/wru-womens-health-initiatives/
- Kenne, K.A., Wendt, L. & Brooks Jackson, J. Prevalence of pelvic floor disorders in adult women being seen in a primary care setting and associated risk factors. Sci Rep 12, 9878 (2022)
- Ng, H. H., Shen, M., Samuel, C. S., Schlossmann, J., & Bennett, R. G. (2019). Relaxin and extracellular matrix remodeling: Mechanisms and signaling pathways. Molecular and cellular endocrinology, 487, 59–65. https://doi.org/10.1016/j.mce.2019.01.015
- Notenboom-Nas, F. J. M., Knol-de Vries, G. E., Beijer, L., Tolsma, Y., Slieker-Ten Hove, M. C. P., Dekker, J. H., van Koeveringe, G. A., & Blanker, M. H. (2022). Exploring pelvic floor muscle function in men with and without pelvic floor symptoms: A population-based study. Neurourology and urodynamics, 41(8), 1739–1748. https://doi.org/10.1002/nau.24996
- Peinado-Molina, R. A., Hernández-Martínez, A., Martínez-Vázquez, S., Rodríguez-Almagro, J., & Martínez-Galiano, J. M. (2023). Pelvic floor dysfunction: prevalence and associated factors. BMC public health, 23(1), 2005. https://doi.org/10.1186/s12889-023-16901-3



